Inflammation in Fascia causes pain – new discoveries presented in Stockholm
- In a sedentary service society and an increasingly digitized world, more people suffer from back and neck problems; problems that lead to impaired quality of living and longer sick leave.
- In recent years new research (Gordh et al 2011, Mense et al 2015, & Wilke et al 2017) shows a direct link between pain and inflammation of the tissue (Fascia).
- Inflammation is the body’s natural way of healing but if continued, inflammation will result in pain. Drawn-out inflammation may have many causes like: poor diet, a sedentary lifestyle, a healing process that has gone wrong, or repetitive, monotonous movements (e.g. tennis elbow).
- Dr Heike Jäger, Professor Karl Arfors and innovator Hans Bohlin presented the latest research regarding Fascia, inflammation and Fascia treatment in Stockholm, May 2017.
“In the beginning it was just great to see how people got well, but why did they? That’s when we started to pay attention to connective tissue.”
Innovator Hans Bohlin and Atlasbalans look for new ways to help people improve based on new research on Fascia/connetive tissue.
Why is this interesting and why is it still relatively unknown?
Extensive efforts have been made to address problems with lower back pain. In 2013 the Swedish Board of Corporate Health Advisors put together the report “Riktlinjer för ländryggsbesvär” (only in Swedish) without really having found the cause for back problems or having answered the question as to why we get back pain.
Perhaps we have to ask new questions to get new anwers?
When innovator Hans Bohlin and professor Karl E Arfors read the report 2014, they instinctively felt that maybe the Board of Health Advisors had overlooked some perspectives which could provide another basis for explanation.
After reviewing and compiling new anatomical research, an alternative explanatory model is starting to form, opening up to new fascinating possibilites.
During spring of 2017 the foundation of this new explanatory model was made into an animation – visualizing how new research changes our perspective on aches and pains. Have a look here:
Fascia treatment & inflammation
Fascia treatment with the machine M1 is innovative way to treat connective tissue and muscle tension, reducing inflammation and increasing mobility.
Treatment results from approximately 400 therapists in Sweden, the EU and the US indicate that inflammation-related disorders are alleviated or completely overcome.
Many people who have been treated, experience reduced problems with back and neck pain. Fascia wave treatment in horses, have led to trotting horses running faster and jumping horses, to a greater extent, remaining injury free.
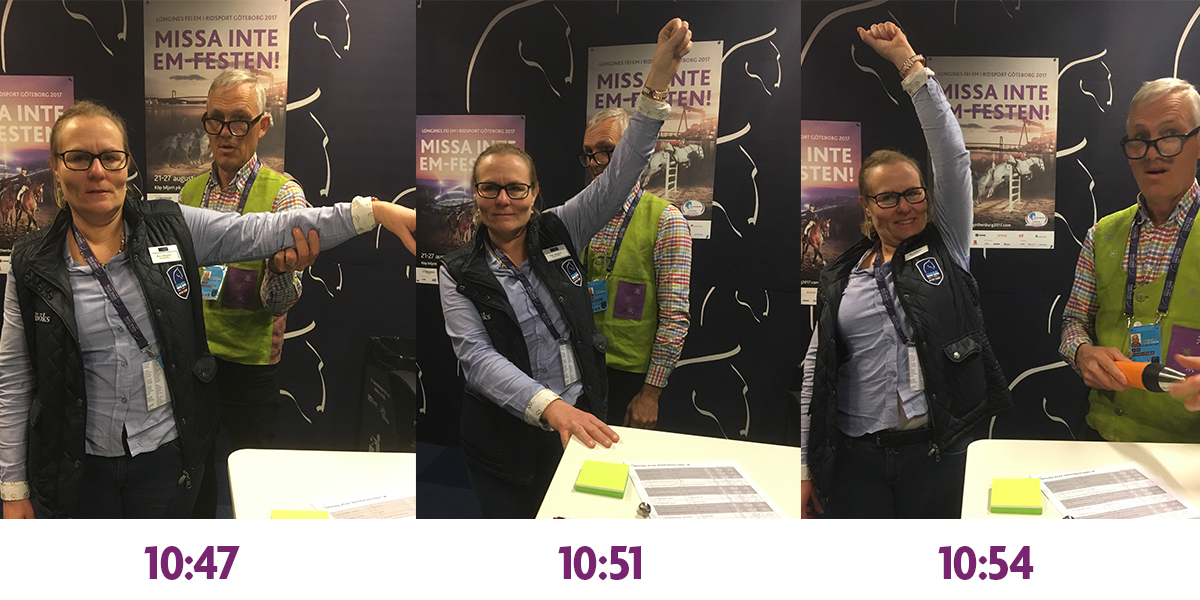
Frozen Shoulder – Tissue Inflammation
A frozen shoulder begins with pain and stiffness of the shoulder that eventually freezes and leads to impaired mobility; a development that takes several months. There are indicators that self-healing is possible, which usually takes one to three years (source WebMD).
New research has found that frozen shoulder is related to tissue inflammation and through Swedish Fascia Vibes several people with frozen shoulder problems have been helped. For many years Åsa used to have problems with a frozen shoulder until she was helped with Swedish Fascia Vibes.
A Collaboration Between Some of Europe’s Leading Experts
Dr. Heike Jäger, Fascia Research Group, University of Ulm
Dr Heike Jäger, neuro physiologist and specialist in muscular deseases, chronic pain and back ache at the Fascia Research Center at the University of Ulm, Germany.
Since the 90s Dr. Jäger has been conducting groundbreaking research on Fascia and problems in the lower back region, with the help of ultrasound and new measuring methods. Together with her colleagues she challenges conventional beliefs about the human body and sets a new standard for anatomical research.
Parts of this research are presented in a German documentary from 2013, where Dr. Jäger also participates. A shorter version of this can be found here.
Professor Karl E Arfors, Honorary Doctor, Uppsala University
Professor Karl E Arfors is Honorary Doctor at the University of Uppsala. He has dedicated most of his research years studying inflammation and microcirculation.
With solid knowledge and experience professor Arfors wants to share with others how to live sound and healthy lives.
After 80 years’ of life and research experience, professor Arfors is prepared to question old knowledge and embrace new ideas and perspectives.
Hans Bohlin, CEO Atlasbalans
Hans Bohlin is a Swedish innovator and founder of Atlasbalans.
In 2010 Hans started asking questions such as “Why do people get recurring problems in the lower back?”; “What is the underlying cause?” – and was very surprised at not being able to find answers.
Perhaps it is Hans’ business background and perpetual driving force to simplify and streamline that has lead to new questions and perspectives. What is certain, however, is that he’s never given up searching for answers. Through the years Hans has probably read more research papers (about 500) than any other Swedish business entrepreneur.
“Hans Bohlin has such original thoughts, he is not tainted by old perspectives, always asks unusual questions and finds interesting associations” – Professor Karl E Arfors
More about Inflammation and Autoimmune Inflammation
Inflammation has a very important function in healing and treating infections. Heat and pain arise and the immune system works actively in dealing with bacteria and healing wounds. Pain also signals that a part of the body is overworked and needs rest. So far inflammation is most normal and important to the healing process.
Autoimmune inflammation, on the other hand, should be looked upon with great concern. This is when the immune system is overactive and starts triggering inflammation randomly in the body. We either inherit the propencity for developing autoimmune inflammation or it is due to life style choices. Certain diets result in a hyper immune system, where the body will start searching for something to attack. A common problem is sugar, which is known to activate inflammation.
Protein in milk and gluten (from wheat, corn, oats and rye) can leak into the body through the intestine and cause the immune system to start a general inflammation. There are theories about gluten causing autoimmune hypothyroidism, since the tissue of the thyroid gland is reminiscent of the gluten protein. If the body has been “trained” to react to gluten, it could very well start attacking the thyroid gland.
Fatty acids from Omega 3 suppresses the inflammation and fatty acids from Omega 6 triggers it.
We get Omega 6 from grains, therefore any kind of food containing wheat and grit increases the level of inflammation. Omega 3, on the other hand, is a protector but can be tricky to get enough of; this fatty acid has a tendency to go rancid.
One study showed that organic eggs contained large amounts of Omega 3, especially if the hens had been fed flaxseeds. The “factory produced” eggs contained next to no Omega 3.
An inflammation may become chronic in an area that has been injured and not have had the chance to heal properly. If for example a muscle starts cramping and the nervous system doesn’t let go, the function of that area will continue to deteriorate and healing will become more and more difficult. In such an area inflammation can lay latent for a long time. If the area is treated healing will begin, resulting in normal function and circulation.
If the inflammation is the result of an overactive immune system, caused by an autoimmune disease (e.g. Thyroid Disease, Rheumatoid Arthritis and Diabetes), problems will most likely return within short.
Conclusion
We can conclude that inflammation may be difficult to understand and treat. A body with a low general inflammation level will be more resistant, and not as easily causing inflammation to joints and muscles as someone with an overactive immune system.
Some people can hurt terribly after just a walk, sensing pain and inflamation of hip joints and knees. Others can strain the body hard and only experience a mild work-out sorness of the muscles.
To be able to give advice to clients who are not easily treated, it is advicable to get familiarized with how inflammation occurs. Clients simply won’t get well if “something” constantly triggers inflammation, causing the body to react to strain.
Of course we can not rule out all sorts of strain on our bodies. In fact, bodies need to be exercised and exerted in order to build strenght and keep flexible. But with a high general inflammation level, a person will not be able to take the slightest strain without hurting.
Exercise and inflammation is not a good match; rather abstain from strain until the inflammation is gone. Pain is a helpful indicator to assess level of inflammation, as is heat and swelling.
Most often inflammation goes away when we treat it and increase mobility and circulation. With a hyper immune system the body is likely to build up new problems after a while. Please point this out to the clients in order to set their expecations right regarding the treatment.